Cleft lip and cleft palate are among the most prevalent congenital disabilities affecting children in Malaysia. The reported incidence of cleft lip and palate is about 1 in 700 live births. Cleft lip (separation of the upper lip) and/or cleft palate (separation of the roof of the mouth), occurs due to failure of fusion of these structures during the early stages of fetal development. The spectrum of these oro-facial deformities may present as a mild form (small indentation on the lip) to an extensive deformity involving the lip and palate of either one or both sides of the face.
The management for cleft lip and cleft palate involves a multidisciplinary team approach, performed at specific age group to correct the structural and functional deformities of the oro-facial region to improve the facial aesthetic, speech, dental occlusion and child’s self-esteem. This multidisciplinary team consists of the plastic surgeon, pedodontist, orthodontist, ENT surgeon, speech therapist, psychologist and nurse. The team can work together to define a course of treatment at a specific age, including surgical repair of the cleft, speech rehabilitation and dental restoration. The timing of management depends on the individual circumstances of the cleft child.
The schedule for the management of cleft patients are as follow:
- Birth to 1 month: plastic surgeon & orthodontist – counselling & presurgical orthopaedic
- 3 to 6 months: plastic surgeon – cleft lip surgery
- 6 to 9 months: plastic surgeon – cleft palate surgery
- From 1 year onwards: speech therapist & ENT surgeon – speech assessment and education
- From 3 years onwards: pedodontist/ dentist – counselling and dental health care
- From 7 years onwards: plastic surgeon – correction of any residual or scar deformities
- 9 to 11 years: plastic surgeon – alveolar bone grafting
- From 11 years onwards: orthodontist – orthodontic management
- 18 to 21 years: plastic surgeon – orthognathic surgery
Surgical reconstruction of a cleft of any kind is a highly individualised procedure intended not only to close the defect but also to ensure that the affected child will be able to function and grow normally.
The timing for cleft lip and cleft palate surgery depend on several factors:
- Age of the child – at least ten weeks of age
- Weight – at least 10 pounds
- Haemoglobin level – at least 10 gm/dl
- Other associated congenital deformities or health status of the child.
The timing for cleft lip surgery or cheiloplasty is usually about 3 – 6 months of age for a healthy cleft child. This surgery consists of:
- Closure of the cleft resulting in a scar located in the normal structures of the upper lip
- Formation of a cupid’s bow (the curve at the centre of the upper lip)
- Considerations for the adequate distance between the upper lip and nose.
In cases where the cleft lip/ palate affects the shape of the nose, additional procedures may be recommended to:
- Achieve symmetry between the nostrils
- Create adequate length of the columella (the tissue that separates the nostrils)
- Increase the angle of the nasal tip, to avoid a flattened nasal tip or one that pulls downward.
Case No. 1

Case No. 2

Case No. 3

Case No. 4

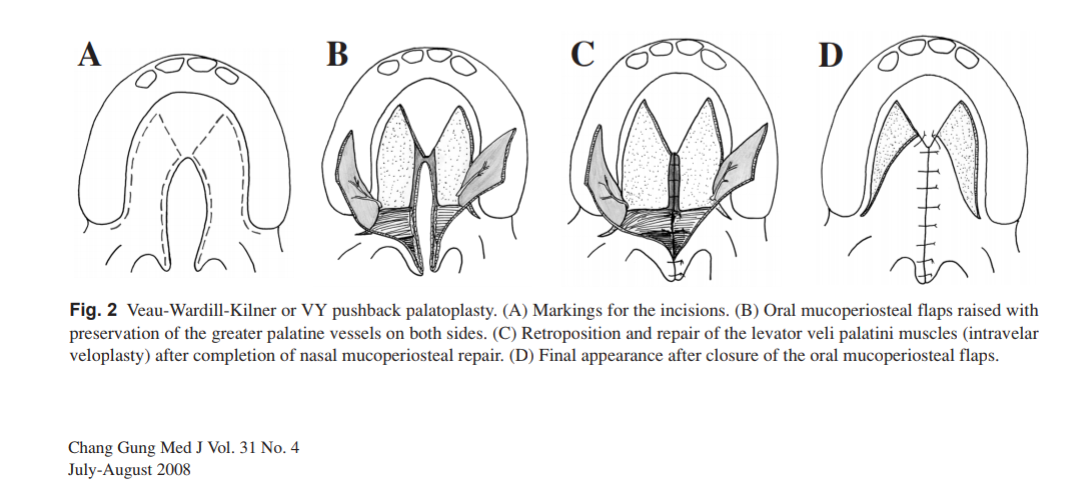
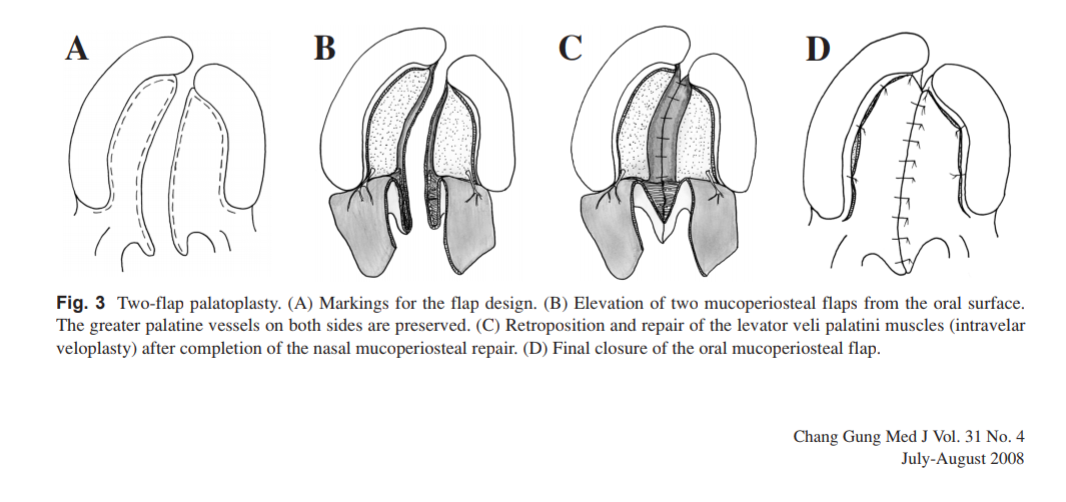
The surgery for the cleft palate (palatoplasty) is usually carried out when the child is about 6 – 9 months of age. The purpose of cleft palate surgery is not only repairing the cleft palate but also to preserve the speech function and allow normal oro-facial growth in later life.


Preoperative evaluation
Communication is vital to achieve desirable goals. During the initial consultation, parents will have the opportunity to discuss with the plastic surgeon about the treatment plan. The plastic surgeon will work closely with the parents to reach an agreement about the expectations from the surgical procedures involved and their long term benefits for their cleft children. Every patient is different. Therefore a specific treatment regimen is planned to suit an individual’s need. The preoperative evaluation includes:
- Discussion about the treatment plan and schedule
- Available surgical options for cleft patients
- The child’s medical conditions, drug allergies and previous medical or surgical treatment
- Discussion on anaesthesia and its risks
- Discussion on the likely outcomes of the procedure and any risks or potential complications
- Physical examination
- Photography for preoperative and postoperative evaluation
Preparation for surgery
- Before scheduled surgery, parents will be given specialised feeding bottles to help them to feed the child and keep up the child’s body weight
- Pacifier or teats will be discouraged
- Preoperative medical evaluation and blood investigations will be done a day before the surgery
- Special instructions will be given on the day before and after surgery
The risks and safety information on surgery
The decision to have cleft surgery is extremely personal. Patients have to consider if the benefits will achieve their goals, and if the risks and potential complications are acceptable. Therefore, it is essential for parents to understand that every surgical procedure has its complications and downtime. However, if a cleft child is appropriately assessed before the surgery and postoperative care is given adequately, these risks can be eliminated or reduced.
Some of the common risks of cleft surgery:
-
- Infection
- Bleeding
- Poor wound healing
- Irregular healing of scars including contracture (puckering or pulling together of tissues)
- Residual irregularities and asymmetries
- Skin discolouration
- Skin contour irregularities
- Skin sensitivity
- Swelling due to a blood clot or fluid accumulation
- Injury to deeper structures such as nerves, blood vessels or muscles
- Anaesthesia risks
- Possibility of revision or staged surgery.
Postoperative expectations
After the surgery, dressings or bandages may be placed on incisions outside the child’s mouth. Special instruction will be given to parents on wound care, medications to apply or to take orally to aid healing and reduce the risk of infection, appropriate feeding method, specific concerns to look for in the general health of the child, and when to follow-up with the plastic surgeon. Occasionally, the child’s arm will be restrained during the recovery period to prevent injuring the operated sites as it heals. Sutures over the upper lip will be removed about 5-7 days after the surgery, whereas the stitches in the palate need not be removed as they will resolve with time. If the child’s nose is repaired during the cleft lip surgery, parents are advised to wear the nostril retainer for the child for 1-2 months to maintain the shape of the nostrils. As the swelling resolved, the healing will continue for several weeks. Regular application of sunblock and scar gel to the operated sites (upper lip) can prevent the formation of irregular scars.
The outcome of the child’s initial cleft lip and/or cleft palate surgery will make a vast difference in the child’s quality of life, ability to breathe, eat and speak. However, secondary procedures may be needed for functional reasons or to refine appearance. Even though the scars of a cleft lip surgery are generally located within the natural contours of the face, they will always be visible.
Postoperative care
- Regular application of prescribed ointment and cleaning the surgical wound as instructed
- Avoid excessive sun exposure during the healing phase
- Proper use of sunscreen on the scar area
- Application of topical scar gel and massage around the scar area will improve the appearance and texture of the scar.
How much will a cleft surgery cost?
Cost is always a consideration in elective surgery. The cost of cleft surgery can vary widely.
The cost of cleft surgery may include:
- Surgeon’s fee
- Hospital or surgical facility costs
- Anaesthesia fees
- Medical tests and
- Prescriptions for medication.
In Malaysia, most of the private health insurance companies do not cover cleft surgeries and their related complications.
